Although Halloween is an enjoyable holiday and celebration for many, there are an increased number of dangers to pets that are particularly prominent at this time of year.
We have discussed chocolate on numerous occasions, however this is the number one toxin that is seen in emergency practices – it is a topic you can never be too familiar with.
The Symptoms
Theobromine (found in chocolate) mainly affects the heart, central nervous system and kidneys. Symptoms will occur from 4-24 hours after the dog has ingested the chocolate and will vary depending on the amount of chocolate (theobromine) the dog has eaten.
- Restlessness and hyperactivity
- Diarrhoea
- Vomiting
- Rapid breathing
- Muscle tension, inco-ordination
- Increased heart rate
- Seizures
How much chocolate is too much?
The VetsNow Chocolate Toxicity Calculator for Dogs is a useful tool.
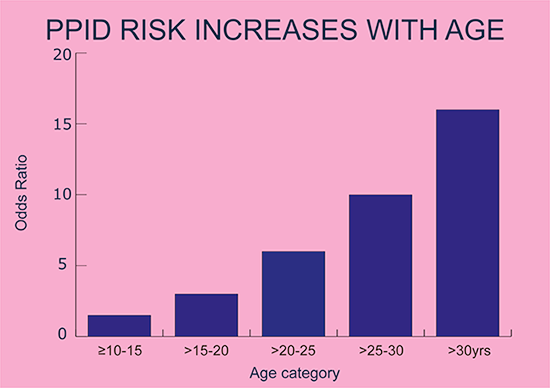
The symptoms of poisoning vary depending on the size of the dog and the amount of chocolate eaten – the larger the amount of chocolate eaten, the more severe the symptoms tend to be. However, signs of toxicity can occur with small amounts of ingestion. For example, this is how chocolate is likely to affect a dog weighing 30kg:
- Ingestion of 200g of milk chocolate is likely to cause a digestive upset (vomit and diarrhoea).
- If the dog had eaten 500g of milk chocolate, it is likely that cardiovascular problems would occur (increased heart rate)
- If the dog has eaten 750g of milk chocolate, it may experience seizures.
How do we treat chocolate toxicity?
The following steps are taken:
- Identify how much chocolate the dog has eaten – look out for empty wrappers as these can be a useful indication. The type of chocolate and the time it was consumed are also important factors in identifying whether the dog has eaten enough to be a toxic dose and what treatment should follow.
- There is no antidote to theobromine. Depending on the timeframe, in most cases inducing emesis with apomorphine will aid in retrieving some of the ingested chocolate. Activated charcoal may also be used to absorb any chocolate remaining in the intestine. In more severe cases, intravenous fluids may be necessary as well as close monitoring of mentation, heart rate, blood pressure and kidney function.
- With prompt intervention and treatment, the prognosis for a dog who has experienced chocolate poisoning is often positive.
Top tips for managing chocolate toxicity cases successfully
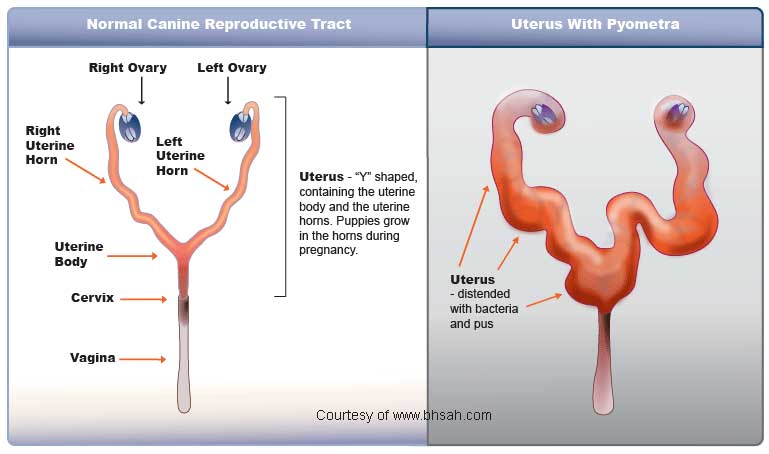
- Don’t forget about the packaging – was this also ingested? Could this cause a risk of GI obstruction?
- Chocolate can be an additional ingredient in seemingly innocuous food items (e.g. cakes, protein supplements) so make sure you check the list of ingredients.