BVD (Bovine Viral Diarrhoea) is a complicated virus that costs the UK cattle industries an estimated £50-75m per year.
Check out our fact sheet below, or you can click here to download it.
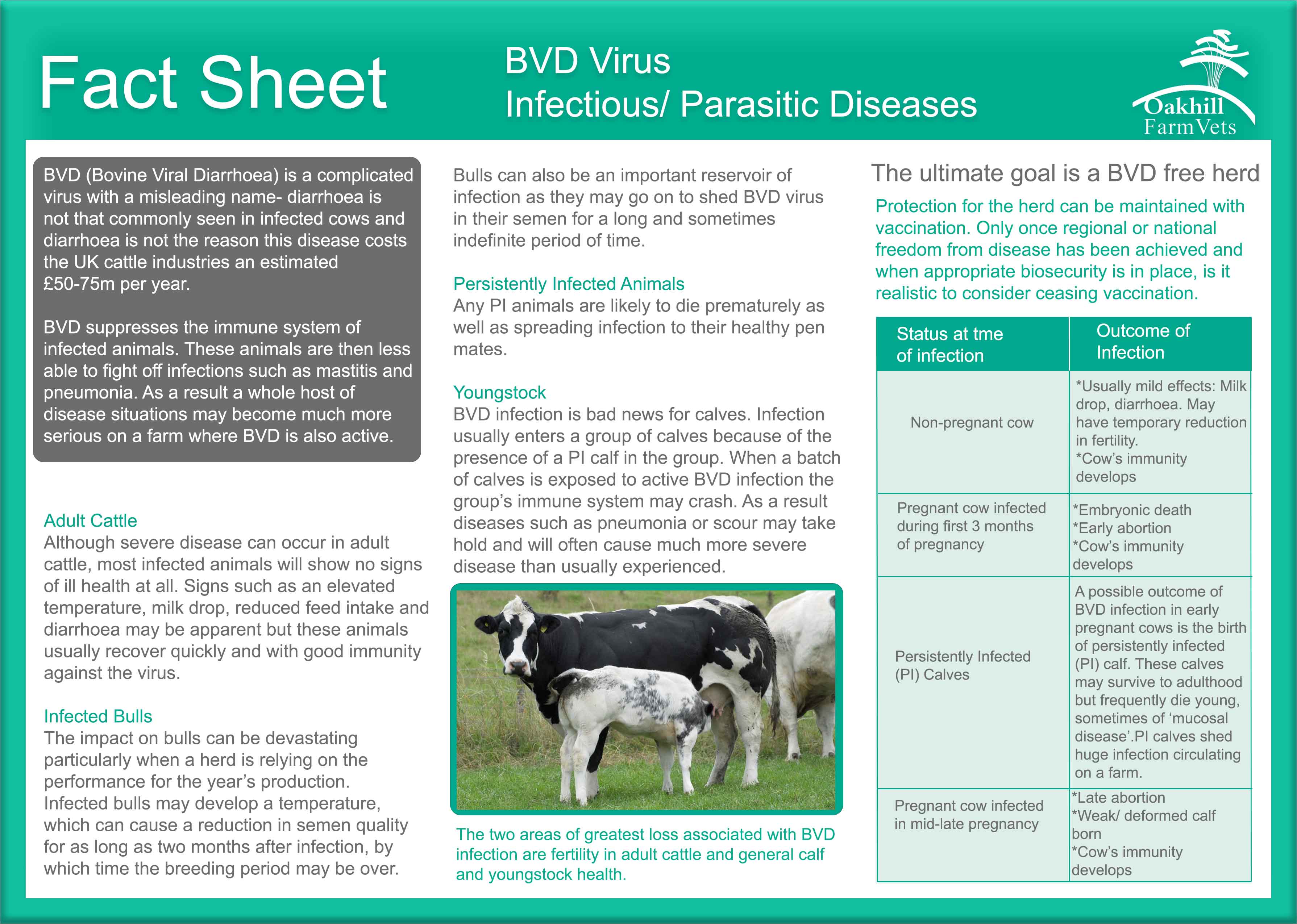

Check out our fact sheet below, or you can click here to download it.

Good fertility management is a key component of successful dairy herd management. Improving herd fertility allows you to sell more milk per year and also reduces the number of cows being involuntarily culled for fertility problems.
The associated costs of poor fertility are highly significant and include:
There are a huge number of factors that influence herd fertility ranging from herd nutrition, infectious disease control, lameness etc. However there are some ‘fertility specific’ areas we can also focus on to improve herd performance. These might include:
We also recommend setting aside some time on a quarterly basis to study fertility performance. These visits allow us to look at what changes we can make to improve fertility and also to quantify any improvements we have made since the previous review. Setting simple targets such as the ‘Number of Cows In-Calf Per Month’ can really help everyone in the farm team focus on improving herd fertility.
Embryo transfer- repeat breeder embryos (‘cow stoppers’)
What is a Problem Breeder Cow?
Cows that have had three or more services at regular (21-24 day) intervals and that are still not in calf.
What treatments can we use to treat problem breeders?
Problem Breeder Embryos – implanting a beef cross embryo 7 days after service in problem repeat breeder cows improved pregnancy rates by over 20% according to a recent UK study.
How does implanting an embryo help?
By implanting a second embryo into the cows’ uterus the strength of the hormonal signals within the cow are doubled and so the likelihood of the cow reabsorbing the embryo(s) is reduced.
What cows would make good Embryo Transfer candidates?
What is the procedure?
Maximising success rates in embryo transfer
These are some suggestions when dealing with embryo recipients.
Lameness
Healthy feet programme
An understanding of which types of lameness are present, coupled with a structured approach to tackle the underlying causes is required to tackle lameness effectively.
The AHDB Dairy Healthy Feet Programme is a structured approach which will help make important progress towards diagnosing the problems, devising an action plan, and develop the skills necessary for long-term lameness control. The approach is based around the ‘four success factors’ – Low infection pressure – Good horn quality and hoof shape – Low forces on the feet – Good cow comfort and cow flow – Early detection and prompt, effective treatment of lame cows
Foot trimming training days
We offer hoof trimming training days that cover the 5-step foot trimming technique, recognition, treatment and prevention of foot lesions in cattle. Watch out for announcements about our foot trimming courses.
Our next foot trimming April 5th, to book onto the 1 day course, please call 01772 861300 or contact farm@oakhill-vets.com.
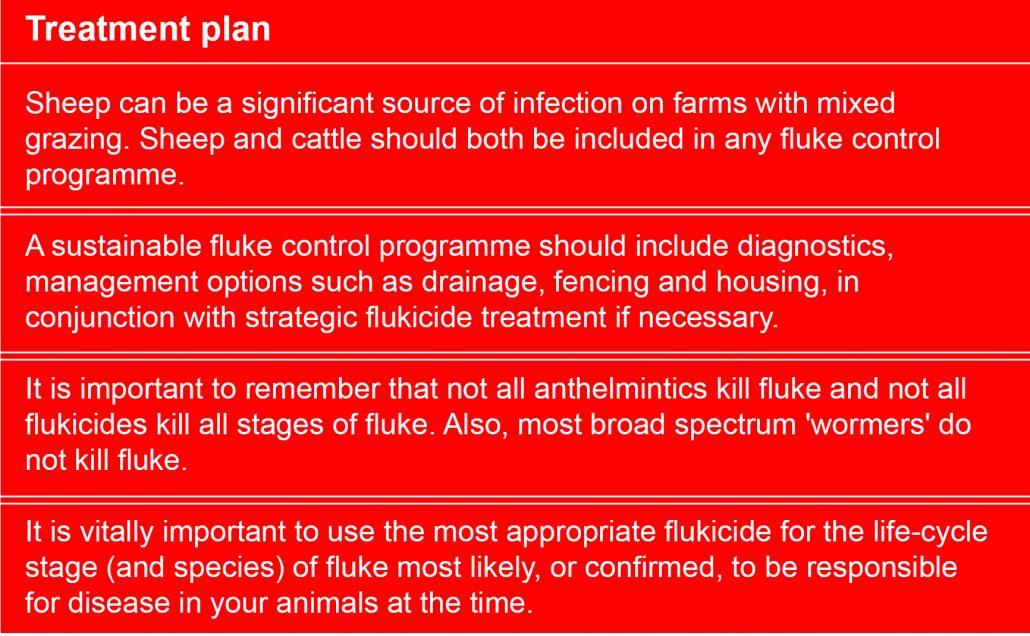
Traditionally Liver fluke was thought to be very regional however movement of stock, changing weather patterns and ground conditions have increased the fluke risk to the whole of the UK. Lancashire has a climate that favours the snail and therefore also favours fluke transmission and increase fluke risk.
A move to housing dairy cows all year round may be thought to remove the risk of Liver Fluke from the herd, but positive bulk milk samples are still reported from zero grazing herds! Where heifers are turned out they may become infected and maintain a reservoir of infection. Where fluke is identified these animals should receive appropriate treatment. Sheep, deer, hares, geese and horses can all carry fluke and complete the lifecycle outside of the snail.
New research by the Mordun Institute has found that Metercerariae (the stage passed by the mud snail that are ingested by cattle) are very persistent and this stage of fluke can survive in silage. Heat and pH are thought to be involved in killing off the Metercerariae in most cases, but in less well fermented silage, wet silage and less acidic silage this is less so. With this in mind poorly made silage, later cuts and big bale silage pose the highest risk. Last year’s silage crops were certainly made in challenging conditions.
Further investigations into housed youngstock infections, egg survival and spread in slurry are ongoing but if you have history of fluke infections in housed cattle submitting further investigation may be useful.

Even in herds that are housed 365, there is still a risk of liver fluke. There is an inexpensive bulk milk test available, some interpretation is needed if first lactation heifers are introduced after grazing. However there is a test available (the coproantigen test) that will test for current infection to differentiate this. It is also thought that Liver fluke can survive in cattle for 2 years.
![]()
Due to the complex life cycle and products available to treat lactating cattle, treatment is often targeted at dry cows often making it difficult to treat the correct animals at the correct stage of infection. Creating a testing and treatment plan with your vet is the best course of action on an individual farm basis. Care should be taken to select appropriate treatment product for dairy cattle, flukicide residues are increasingly being detected in bulk milk samples.
Randox Foods have created an ELISA test that can detect antibiotics, anti-inflammatory and anthelmintic in milk, which is used alongside the industry standard DELVO test by DAIRY UK to detect veterinary residues in milk.
Dairy UK along with vets and other industry members have created MilkSure to decrease the likelihood of bulk tank failures due to residues. This educational tool is provided by your veterinarian and involves a training course, risk assessment and online exam.
Katherine is our trained MilkSure vet and is on hand to answer any questions relating to this, feel free to email us with any enquiries to farm@oakhill-vets.com.

 The NADIS liver fluke forecast for the end of 2017 held true with many flocks in Lancashire being exposed to a heavy burden of fluke.
The NADIS liver fluke forecast for the end of 2017 held true with many flocks in Lancashire being exposed to a heavy burden of fluke.Both acute fluke and sub- acute fluke were prevalent so treatments administered were targeting immature fluke. The products used were either triclabendazole and/or closantel and/or nitroxanil depending on the flocks’ history. While these products are very effective, repeated use will inevitably increase the risk of resistance, to the active ingredient.
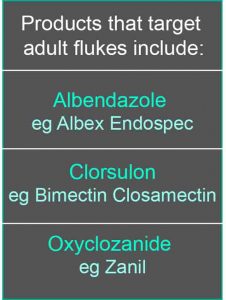
To limit resistance, other flukicidal products should be considered, now that the main risk period is coming to an end. Paddocks grazed over the autumn and winter will now carry a much lower burden of the infective metacercariae so treatments can be targeted at the adult flukes (Chronic fluke) that have survived. Targeting the adult fluke at this time of year will reduce the number of fluke eggs shed onto pasture before the mud snails become active.
If you would like anymore information, please contact us.
It is of paramount importance that these horses/ponies do not come out of Winter carrying even more weight! We want these horses to have achieved a ‘normal body condition score’ prior to turn out on Spring grass. Overweight equids should ideally be fed good quality hay as this is less calorific than haylage.
We should aim to feed 1.5% of body weight in kilograms of hay, weighed dry, per day. Hay can be soaked for ideally 8-12 hours before feeding to reduce the non-structural carbohydrate load. If feeding soaked hay, a low-calorie vitamin/mineral balancer should also be fed. Remember any dietary changes should be made gradually over a 2-week period to try prevent gastrointestinal upset. Furthermore, overweight horses/ponies should not be over-rugged. Unclipped, overweight horses/ ponies not in work, do not need rugging!
On the flip side of the coin some horses, especially our older patients, can struggle to maintain condition in winter. These patients should have regular dental checks performed as well as being subscribed to a veterinary devised worming programme.
Furthermore, such patients benefit from an increased plane of nutrition as well as adequate rugging. Blood tests including ‘Cushing’s’ bloods should also be considered in such patients.
If you’re worried about your horse’s weight, please contact us.
Horses come in all sorts of different shapes and sizes, and like humans they can gain weight, which can lead to other health issue.
Obesity in the horse world is as common a problem as it is in the human one, with the weight gains occurring when a horse’s nutritional intake exceeds his physical output. Basically, if your horse is eating more than he’s burning off, he’ll get fat.
All horses, whether ridden or not, stabled or living out, will need to have their diet, health and exercise managed in accordance with their type and workload to ensure they maintain a healthy weight.
Overweight horses are prone to developing various health problems including chronic laminitis, oxidative stress and a less than perfect interaction between insulin and blood glucose. While obesity itself may not directly cause these problems, it certainly has some relationship to the metabolic processes that keep body tissues and systems healthy.
Furthermore, the excess weight a horse carries leads to heat stress, strain on joints and connective tissues and reduced levels of performance.
It’s a good idea to check your horse’s weight regularly either using weigh tape, or if you’re on our Equine Care Plan Premium, you’ll have access to our weight bridge to accurately measure your horse’s weight.
If you’re concerned about your horse’s weight or unsure of what weight they should be, please contact us and one of our vets will be able to assist and advise you.