Toby, a 7 year-old, Cob cross pony presented to Oakhill with a several week history of mild, right forelimb lameness. Despite a short period of box rest and pain-relief, the lameness did not resolve, and a veterinary opinion was sought.
Nikki Platt, our senior lameness veterinary surgeon examined the pony and noted that the pony’s front feet pointed in slightly, and that the outer walls of his hooves were slightly longer than the inner walls. When observed moving, Toby was sound in a straight line, 3/10 right forelimb lame on the left rein and 2/10 right forelimb lame on the right rein. The lameness was slightly more obvious on a firm surface. The pony did not resent standing with his limbs flexed up, and this procedure (known as a flexion test) did not cause any increase in lameness.
In order to be certain of the origin of the lameness, diagnostic analgesia was performed (where local anaesthetic is used to remove pain sensation from an area). A palmar digital nerve block was used to de-sensitise the right foot. This caused the resolution of the right forelimb lameness, and the appearance of a mild left forelimb lameness was present when the horse was lunged. It is common when performing diagnostic analgesia that, having eliminated the most significant pain from the lame limb, the horse then begins to show lameness in the opposite limb, as the horse is a symmetrical animal after all!
Having conclusively identified the source of pain, x-rays of the feet were taken. In this case, the bony structures of the foot were unremarkable other than to identify a slight compression of the coffin joint space on the medial (inside) aspect compared to the lateral (outside). The lack of explanation for the cause of the lameness on the radiographs meant a need to assess the soft tissues of the foot by performing MRI (magnetic resonance imaging).
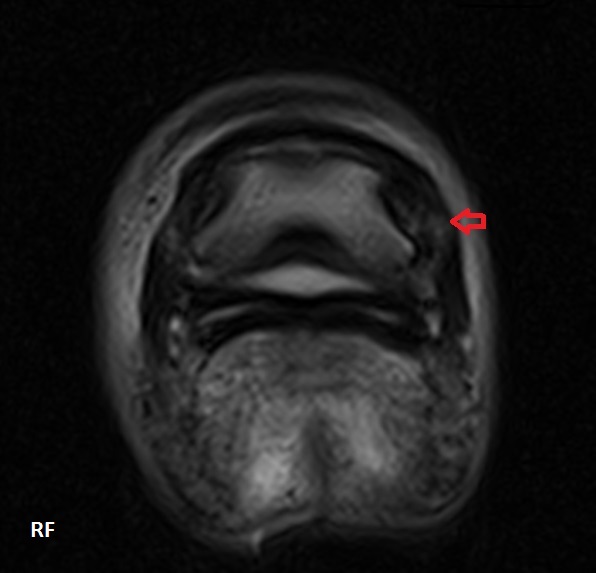
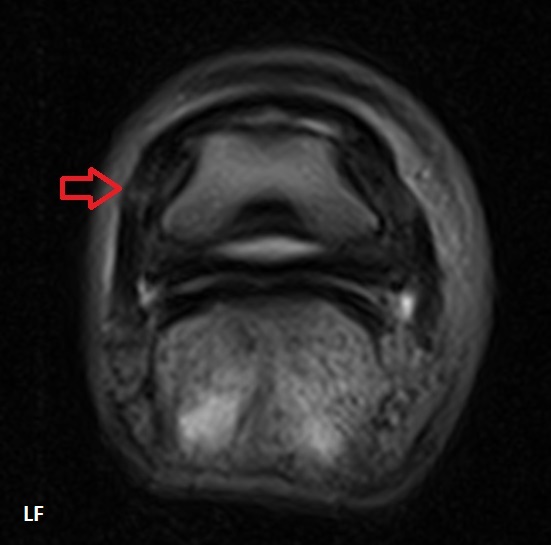
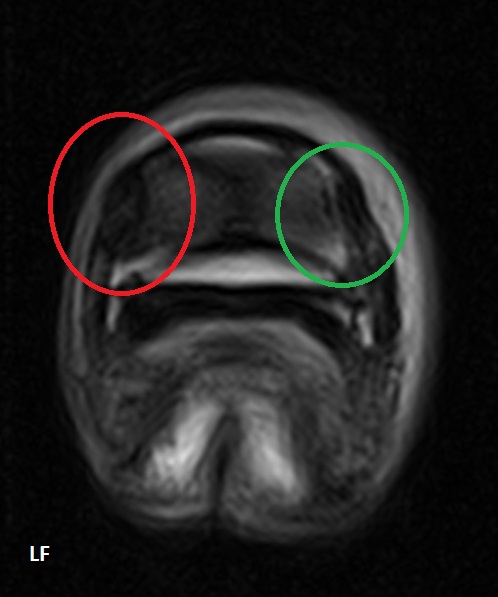
The procedure was carried out under mild sedation with the pony standing. Following the evaluation of the 400+ images of Toby’s feet we obtained, the diagnosis was clear – moderately severe collateral ligament desmitis (inflammation) of the coffin joint in both front feet.
The collateral ligaments are responsible for stabilising the movement of a joint. If (like with this pony’s ‘toe in’ conformation) there is a slight twist in the limb, a joint can be loaded unevenly across its surface during weight bearing. This means that one or both of the ligaments may be subject to more strain than it is designed to take whilst stabilising joint movement. This repetitive, excessive strain leads to microscopic damage of fibres within the ligament, causing inflammation, pain and scarring.
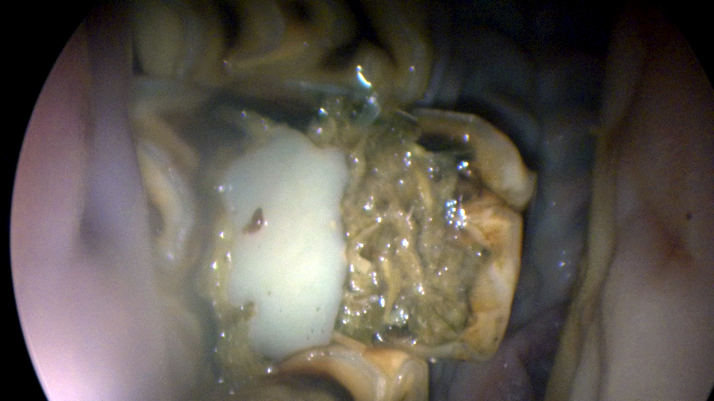
On the MR images pictured, the red arrows and circles indicate the damaged medial collateral ligament (with the green circles highlighting the comparatively normal lateral ligament). The damaged ligaments have an ‘increased signal intensity’ i.e. they have a brighter, whiter appearance, due to the infiltration of inflammatory fluid into the structures. The damaged ligaments are also larger, partly due to this fluid infiltration, and partly due to scar tissue being laid down.
MRI was crucial in this case to reach a diagnosis. In reaching a diagnosis, we were able to advise on appropriate treatment. In the first instance, this horse was prescribed six weeks of box rest with a gradually increasing walk exercise programme. The farrier’s involvement was also crucial in this case – the pony was trimmed to maximise the symmetry of the foot (the farrier was able to work from the radiographs provided) and shod in heart bar shoes to help to stabilise the way it was landing.
After six weeks, the pony was greatly improved, showing just 1/10 right forelimb lameness on the left rein only. Having given the soft tissues adequate time to rest, a low dose of steroid was injected directly into the coffin joint, to resolve the mild inflammation that remained at the margin of the ligaments. One month later, the pony was sound!
Toby is now successfully building back up to his previous level of exercise, and is anticipated to remain sound with ongoing maintenance of good foot balance.