If you’d rather avoid an emergency trip to the vets this Christmas, beware of these Christmas dangers for dogs:


New housing measures to protect poultry and captive birds from avian influenza across England, Scotland, Wales and Northern Ireland will come into force from 00:01 on Monday 29th November.
This means that it will be a legal requirement for all bird keepers to keep their birds indoors and to follow strict biosecurity measures in order to limit the spread and to eradicate the disease.
More information available at:
GOV.WALES: https://gov.wales/new-housing-measures-protect-poultry-and-captive-birds-against-avian-flu-0
DAERA-NI.GOV.UK: https://www.daera-ni.gov.uk/news/avian-influenza-housing-order-come-force-0
In May 2021, under the Action Plan for Animal Welfare, it was announced that the government are considering enforcement of microchipping in pet cats. We’ve prepared answers to some frequently asked questions about microchips.
A microchip is a small computer chip, approximately the size of a grain of rice, that is placed under the pet’s skin, usually between their shoulder blades. The microchip contains a unique number that a vet, dog warden or rescue centre can use to search the national databases for the owner’s details.
The vet, nurse or suitably qualified person will pinch the scruff (loose skin between the shoulder blades) and then use a specialised needle to implant the microchip under the skin. The procedure takes a couple of seconds, and although it can feel a little uncomfortable, most animals quickly forget about the experience and there is no long lasting pain or discomfort. It is important that we do not stroke around this area for around 24 hours, whilst the skin heals, to reduce the risk of dislodging the microchip.
Microchips typically last for a pet’s lifetime. In rare cases, microchips can ‘fail’, and stop working. This is why vets routinely check the microchips of pets under our care; if a microchip fails we implant a new one, with no need to remove the defective chip.
Under current legislation, pet dogs over 8 weeks old must be microchipped, so by law all dog owners must ensure their pets are microchipped. This law doesn’t yet apply to cats, but, as mentioned above, this is likely to become a legal requirement in the near future. Importantly, microchips are the best way to ensure that if a pet becomes lost, we are able to contact you as soon as possible to renuite them with you. In cats, if the cat is involved in an accident away from home, being able to contact the owners as soon as possible is important to discuss treatment plans. In addition, sadly pet theft has increased in recent times, and there are many cases of stolen pets being reunited through their microchips.
Over a pet’s lifetime, it is important to update the database with changes of address and phone numbers. To update the details, you can contact Pet Trac, one of the largest microchip databases (https://www.pettrac.co.uk/). If your pet’s microchip is not registered with this database, they will advise you which database to contact.
As always, please get in touch if you have any questions.
Squamous ulceration and glandular ulceration are considered separate disease entities and whilst the risk factors for squamous ulceration are well publicised, further research is required for glandular ulcerative disease. By knowing the risk factors for ulcerative disease, we can endeavour to develop prevention strategies. In some horses, it is impossible to ascertain the trigger factor but ongoing care with diet, management and reduction in stress are of paramount importance regardless.
As we will have previously discussed, access to fibre, little and often, is very important for the prevention of gastric ulceration. Horses should have access to grazing, ideally with companions, and whilst stabled, receive access to hay/haylage. Many people interpret this as a licence to over feed horses and this is certainly not the case. In those horses that are overweight, the recommended quantity of hay should be divided out over a 24-hour period, ideally as 4-6 feeds and not given as one feed only. Hay may be soaked and double netted to slow ingestion speed.
If feeding bucket feeds, select low starch/sugar feeds. A number of suitable feeds are available and we are more than happy to discuss this with you on an individual basis.
Corn oil has varying scientific evidence and as such goes ‘in and out’ of fashion but may reduce gastric acidity. But remember, corn oil is calorific so may not be suitable if your horse is carrying too much weight as it will result in further weight gain.
Are also considered risk factors for the development of ulceration. Ad lib water should be provided at all times and if using electrolytes, these should be used judiciously and added to feed.
Intense exercise is another risk factor for squamous ulceration. As exercise intensity increases, so does the incidence of squamous ulceration. Remember to feed a handful of hay/alfalfa 15 minutes before work to increase the fibrous matt in your horse’s stomach and in turn, reduce acid splash.
Stress is inevitably a contributing factor to gastric ulceration. Horses are herd animals and as such should have companions and freedom to display natural behaviors including access to turn out alongside their companions.
Stable enrichment should be considered for periods your horse is stabled- stable mirrors, treat balls etc. A number of commercial calmers are also available with varying degrees of success in individual patients.
Lack conclusive scientific evidence but a couple of new products have been released as of late. It is too early to comment on our experiences just yet but watch this space!
Dogs cannot sweat through the skin, and mainly lose heat through panting – if you imagine wearing a fur coat whilst out on a walk it gives some understanding how easily they can develop heatstroke! So as the temperature rises, it’s important to make sure your pets are kept cool and comfortable. There are lots of ways to do this:
Symptoms of heat stroke include agitation, stretching out, panting heavily, drooling, hot skin, glazed eyes, vomiting and collapse.
If you feel your pet is becoming hot try cooling down with damp cool cloth (especially in cats), or a water spray (dogs). If the symptoms persist then please ring us immediately for advice.
And finally, never leave your dog in the car – even on a mild day a car can quickly become an oven, even with the windows open.
As humans, we tend to embrace the sunshine and warmer weather that the summer months bring us. However, enjoying these warmer temperatures can quickly become very dangerous for our four-legged friends. Dogs lack the amount of widespread sweat glands that humans possess; only having sweat glands in their feet and around their nose. Therefore, they are unable to tolerate the heat like we can, relying on panting to keep themselves cool. Brachycephalic breeds (flat-faced breeds) such as Pugs, Bulldogs and Boxers have a further increased susceptibility to heat stroke due to their upper airway abnormalities. We want to make everyone aware of the risk that warmer weather poses so we can enjoy the summer safely together.
The signs that a dog may exhibit can vary as the body temperature rises and heat stroke develops in severity. If you recognise any of the below signs you should seek veterinary advice immediately:
Heat stroke is the result of a dog unable to control his body temperature resulting in hyperthermia. This may be exertional heat stroke as a result of a dog being exercised in warmer temperatures, or non-exertional due to lack of ventilation and/or water which is typically seen in dogs left in parked cars. There is no defined space of time of how long it can take for a dog in a parked car to develop heat stroke, however, this can be as little as 15 minutes.
Tips to help keep your dog safe:
Timing is crucial with these cases; the sooner the signs of heat stroke are noticed by an owner, and the dog receives prompt veterinary treatment, the better the prognosis. Where possible, phoning the veterinary practice in advance of setting off to the vets with your dog can be beneficial; we may well advise you to start cooling techniques before your journey. On arrival, we will assess your pets condition and provide veterinary treatment as needed. This can include applying cooling techniques, administering intravenous fluids alongside constant monitoring of clinical signs. Unfortunately, despite aggressive veterinary treatment, heat stroke can result in serious long term complications such as kidney failure or in some cases can even be fatal.

 Xrays were taken here at our Goosnargh practice and Oakhill Farm Vet, Amy Bowers operated to remove the extra structure. Without removal, the lamb was a risk of it getting caught and sustaining trauma.
Xrays were taken here at our Goosnargh practice and Oakhill Farm Vet, Amy Bowers operated to remove the extra structure. Without removal, the lamb was a risk of it getting caught and sustaining trauma.Chocolate
During Easter we all enjoy eating some (a lot of) chocolate. Whilst for us it is a delectable treat, for dogs (and cats) if ingested, can cause life threatening illness. Chocolate contains theobromine that at toxic levels can cause vomiting, diarrhoea and shaking and can lead onto seizures (fits), heart issues and ultimately death. If you suspect your dog has consumed chocolate please ring the practice immediately as if treated early can reduce the risk to your dog.
Hot Cross Buns (raisins)
Raisins within hot cross buns can cause irreversible kidney failure and sadly death if consumed by dogs. Toxic doses vary and a very small amount can be deadly. If your dog has or even is suspected to have ingested raisins or grapes immediate veterinary treatment is indicated.
Bulbs
Easter is a time when spring emerges and our gardens and hedgerows are bright with colour from flowers. Certain flowers for example daffodils and hyacinths originate from bulbs buried in the ground. Dogs, especially puppies may be dig them up and may chew and ingest them. Toxicities can vary but usual signs of vomiting and diarrhoea are common. Veterinary intervention may be indicated so please contact the practice if you have any concerns.
Lilies
Lilies are highly toxic and extremely dangerous for cats and will cause kidney failure and sadly death. All parts of the lily is toxic i.e. stem, flower and pollen. The most common route of ingestion if through the pollen whilst grooming. Our advice would be to NEVER have lilies in a house where cats are present.
Anti-freeze
As the weather warms and people get out and about into their gardens and garages, cats have access to areas where chemicals such as antifreeze are stored. Antifreeze is sweet and is sadly enticing to cats which if consumed causes irreversible kidney failure. As cats are outdoor animals it can be hard to stop this however owners can alert unaware neighbours to keep chemicals such as antifreeze locked away from prying paws.
Anderson Moores Vet Specialists have confirmed three new cases of the deadly dog disease have been found in the UK, with one case in Preston.
Alabama Rot is a potentially fatal disease affecting dogs which has been identified across most of the UK since 2012. The disease doesn’t discriminate between age, gender or breed and the cause is still unknown.
The disease (also known as CRGV) has been dubbed the ‘black death’ because it’s so aggressive. When it comes to the symptoms, the most obvious are unexplained skin lesions. They are often circular and typically appear on a dog’s lower legs, below the knee or elbow and in rare cases, they’ve also been found on the stomach and face.

The lesions may look like a simple swelling or ulcer and the dogs affected usually lick the wounded area and it will become hairless. The lesions are likely to be followed by kidney failure, which presents symptoms of vomiting, tiredness and lack of appetite, these signs can take up to 10 days to present.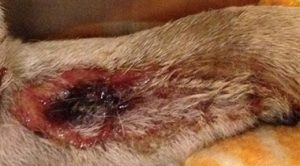
Despite the disease slowly working its way up the country, it doesn’t appear to be contagious as there are no known cases of it spreading from dog to dog. There’s some anecdotal evidence that suggests it could be picked up by pets drinking in the outdoors, although this has not been proven. Another suspect is that it can be caught from muddy and wooden areas as many of its victims were diagnosed after being walked in the woods, this has led vet to ‘strongly suspect’ there is an environmental trigger- possibly a toxin in the muds that the dogs are absorbing on their walks. The issue with this claim is that hundreds of dogs walk in the same areas of the countryside every day and only a tiny number are affected, this could mean those dogs have some intrinsic predisposition to the disease.
As the cause of Alabama Rot is still unknown, developing a vaccine hasn’t been possible. The good news is some dogs have survived after being diagnosed with the disease, if the skin ulcers are present but no kidney injuries are present, the prognosis is good. However around 85% of the dogs affected go on to develop kidney injuries and do not survive.
Time is of the essence with Alabama Rot as it develops incredibly fast, as soon as skin lesions appear, you should get your dog to the vet ASAP as the best chance of success is early, aggressive veterinary treatment.
Although Alabama Rot is a terrifying disease for any dog owner, the chances of your dog catching it are still very slim.
If you’re concerned that your dog may have Alabama Rot, please Contact Us
At Oakhill we see many limping dogs, most of which fortunately resolve simply with rest and pain relief medication. Sometimes however, this is not the case, and rest and medication is not enough.

Tilly, a lovely cocker spaniel cross poodle came to see us at our Kirkham branch as she had been suffering from a sore hind leg causing her to limp. This was not good for poor Tilly as she is a very active and bouncy dog!
After a thorough clinical exam Tilly was diagnosed with very movable knee caps (patellae) that dislocate from their normal position in the groove at the bottom of the thigh bone (femur). This is known as patella luxation which, if serious enough and left untreated, can result in arthritis. It is usually a disease that an animal develops when they are young, due to the shape (or conformation) of their legs as they grow and is influenced by genetics – i.e. can be passed from affected parent dogs. This disease can affect many different breeds of dog (and cats for that matter), however breeds such as Poodles, Chihuahuas, many Terriers and French bulldogs tend to be over represented.
Initially Tilly was treated with pain relief medication and rest however her lameness did not improve. Therefore Tilly underwent x-rays to rule out any other diseases and ensure she was a good candidate for surgical treatment, which she was.

Tom, one of our vets, undertook a surgical technique on Tilly called a tibial tuberosity transposition and wedge sulcoplasty (what a mouthful!) which put simply, deepens the grove the knee cap sits in and realigns part of the shin bone (tibial crest) to pull and keep the knee cap in the correct position. This is done by cutting the shin bone and pinning it in a slightly modified position.
Tilly has had to be kept well rested after the surgery- a hard task indeed! She has done very well and is no longer limping and back to her bouncy happy self.
Reference: O’Neill, D.G., Meeson, R.L., Sheridan, A. et al. The epidemiology of patellar luxation in dogs attending primary-care veterinary practices in England. Canine Genet Epidemiol3, 4 (2016)