Atypical Myopathy is a very serious and often fatal disease that horses can get when out at pasture from consuming sycamore seeds.
What is Atypical Myopathy?
An acute, severe rhabdomyolysis (a severe form of azoturia / tying up) that occurs independently of exercise. The disease causes extreme muscle cramping and often irreparable muscle damage.
Muscle enzymes that are released when the muscles are damaged, cause multiple organ failure.
What is the cause?
A toxin called Hypoglycin-A found in sycamore seeds. Ingestion of these seeds at pasture causes Atypical Myopathy. Outbreaks may occur with multiple horses affected in one geographical area within a few weeks of each other.
What are the clinical signs?
The onset of Atypical Myopathy is acute. Early presentation of the disease may be confused with colic or laminitis. Horses may be found dead, but more frequently they start by showing signs of weakness, stiffness, falling over, lying down more than usual, sweating, apparent sedation or depression, fine muscle tremors, dark brown urine that can look like blood and respiratory distress.
Progression to recumbency is often rapid and once at this stage, the prognosis is hopeless. Mortality is seen in 70% – 90% of cases within 3-5 days.
Who is at risk?
The condition predominantly affects young animals, but all horses are at risk. No sex or breed predisposition has been described, but to date, no cases of the disease have been reported in donkeys. Underweight body condition is associated with increased risk.
Overgrazed pastures and poor quality grazing gives a greater risk of disease.
What can I do to prevent Atypical Myopathy?
Clear fields and water troughs of sycamore seeds, leaves and saplings. If this is not possible, do not allow horses to graze affected paddocks or fence off affected areas. Do not over graze paddocks and avoid overgrowth of weeds on pasture. Provide hay if the fields are low on grass and where possible consider stabling horses over night.
What to do if you think your horse may have Atypical Myopathy
Ring your vet immediately. Try and move the horse to a stable with deep bedding in case they want to lie down. If you notice your horse urinating try and catch a urine sample with a clean jar or mug so that we can test it.

 Pippa, a beautiful Cockerpoo, was diagnosed at 4 months of age with a serious congenital heart defect known as Patent Ductus Arteriosus (or PDA for short) after a heart murmur, that was picked up during her initial vaccination appointment, failed to disappear.
Pippa, a beautiful Cockerpoo, was diagnosed at 4 months of age with a serious congenital heart defect known as Patent Ductus Arteriosus (or PDA for short) after a heart murmur, that was picked up during her initial vaccination appointment, failed to disappear.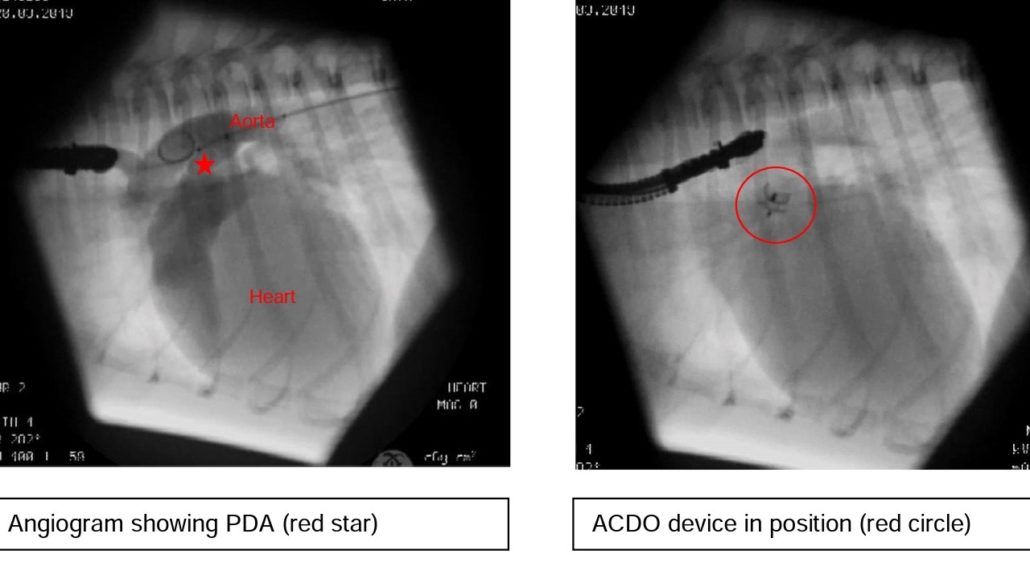
 The procedure has been a complete success so far and Pippa can hopefully now look forward to a completely normal and lengthy life!
The procedure has been a complete success so far and Pippa can hopefully now look forward to a completely normal and lengthy life! The rams will have to work hard during the tupping period and if they’re not on top form fertility is likely to suffer. A general MOT is the best place to start – are the rams healthy and can any problems be corrected? After which, we need to know if they are fertile. Checks need to be made early in the run up to tupping to allow plenty of time to correct any problems.
The rams will have to work hard during the tupping period and if they’re not on top form fertility is likely to suffer. A general MOT is the best place to start – are the rams healthy and can any problems be corrected? After which, we need to know if they are fertile. Checks need to be made early in the run up to tupping to allow plenty of time to correct any problems. • TOES
• TOES


 All RCVS-accredited practices have to meet Core standards, including hygiene, health and safety, clinical governance and the facilities provided. On top of this ‘Core’ accreditation, General Practices can gain species – or discipline-specific accreditations, for example, small animals, farm animals, equine patients.
All RCVS-accredited practices have to meet Core standards, including hygiene, health and safety, clinical governance and the facilities provided. On top of this ‘Core’ accreditation, General Practices can gain species – or discipline-specific accreditations, for example, small animals, farm animals, equine patients.