In May 2021, under the Action Plan for Animal Welfare, it was announced that the government are considering enforcement of microchipping in pet cats. We’ve prepared answers to some frequently asked questions about microchips.
What is a microchip?
A microchip is a small computer chip, approximately the size of a grain of rice, that is placed under the pet’s skin, usually between their shoulder blades. The microchip contains a unique number that a vet, dog warden or rescue centre can use to search the national databases for the owner’s details.
How is a microchip implanted?
The vet, nurse or suitably qualified person will pinch the scruff (loose skin between the shoulder blades) and then use a specialised needle to implant the microchip under the skin. The procedure takes a couple of seconds, and although it can feel a little uncomfortable, most animals quickly forget about the experience and there is no long lasting pain or discomfort. It is important that we do not stroke around this area for around 24 hours, whilst the skin heals, to reduce the risk of dislodging the microchip.
How long do microchips work for?
Microchips typically last for a pet’s lifetime. In rare cases, microchips can ‘fail’, and stop working. This is why vets routinely check the microchips of pets under our care; if a microchip fails we implant a new one, with no need to remove the defective chip.
Should I microchip my pet?
Under current legislation, pet dogs over 8 weeks old must be microchipped, so by law all dog owners must ensure their pets are microchipped. This law doesn’t yet apply to cats, but, as mentioned above, this is likely to become a legal requirement in the near future. Importantly, microchips are the best way to ensure that if a pet becomes lost, we are able to contact you as soon as possible to renuite them with you. In cats, if the cat is involved in an accident away from home, being able to contact the owners as soon as possible is important to discuss treatment plans. In addition, sadly pet theft has increased in recent times, and there are many cases of stolen pets being reunited through their microchips.
My pet is already microchipped, do I need to do anything?
Over a pet’s lifetime, it is important to update the database with changes of address and phone numbers. To update the details, you can contact Pet Trac, one of the largest microchip databases (https://www.pettrac.co.uk/). If your pet’s microchip is not registered with this database, they will advise you which database to contact.
As always, please get in touch if you have any questions.


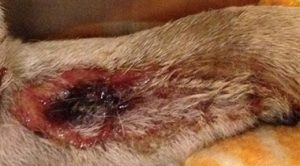
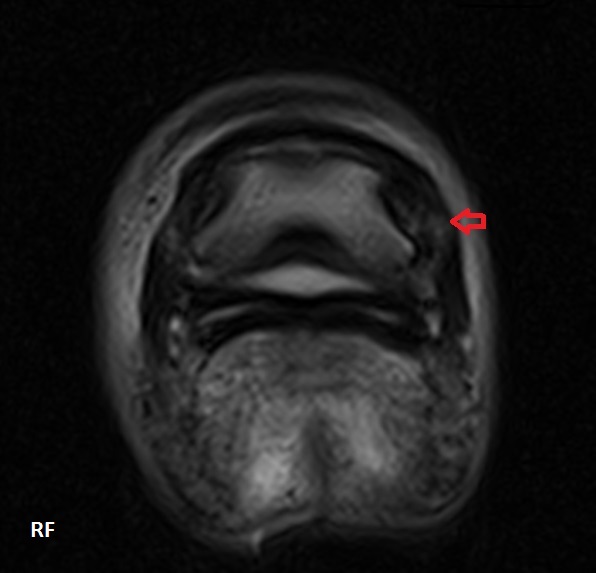
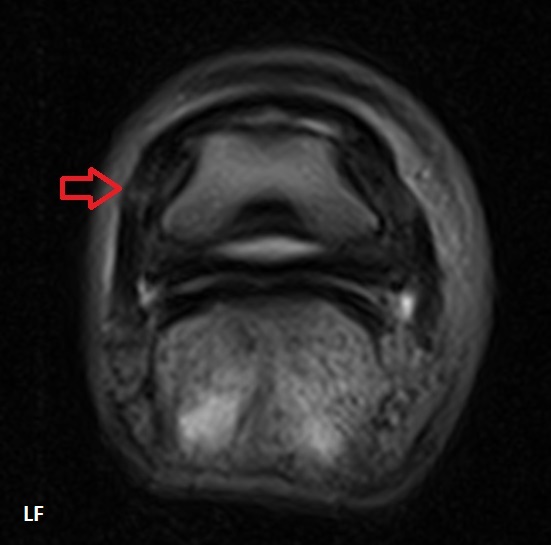
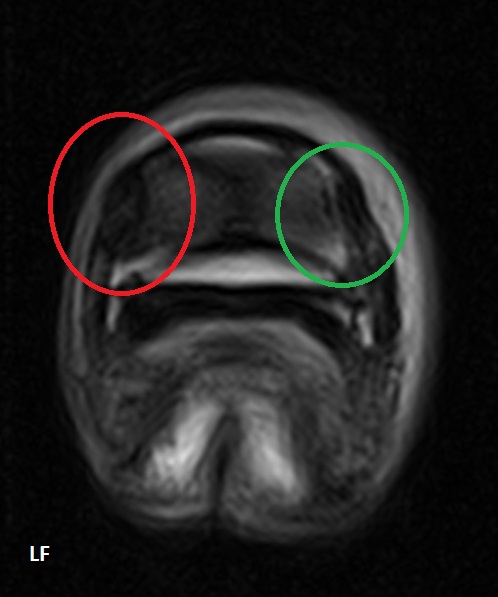
 Xrays were taken here at our Goosnargh practice and Oakhill Farm Vet, Amy Bowers operated to remove the extra structure. Without removal, the lamb was a risk of it getting caught and sustaining trauma.
Xrays were taken here at our Goosnargh practice and Oakhill Farm Vet, Amy Bowers operated to remove the extra structure. Without removal, the lamb was a risk of it getting caught and sustaining trauma.