Infundibular Caries is the name given to a condition affecting the upper molars of some horses. Horses have many adaptations in their teeth designed to help with the rough nature of their diet. One of these adaptations is the ‘infundibulum’.
This is simply an extra area of enamel, one of the hardest compounds found in the body, filled with a softer cementum. Having more of this hard enamel is therefore ideal for grinding down rough tree branches in the wild! Occasionally, the area within this extra enamel doesn’t develop as it should, for reasons that are not completely understood.
The horse is therefore left with a hole within the tooth which fills with food. Over time this food can cause the tooth to rot resulting in either infection of the tooth or catastrophic fracture. You will be pleased to hear that both of these outcomes are completely avoidable!!

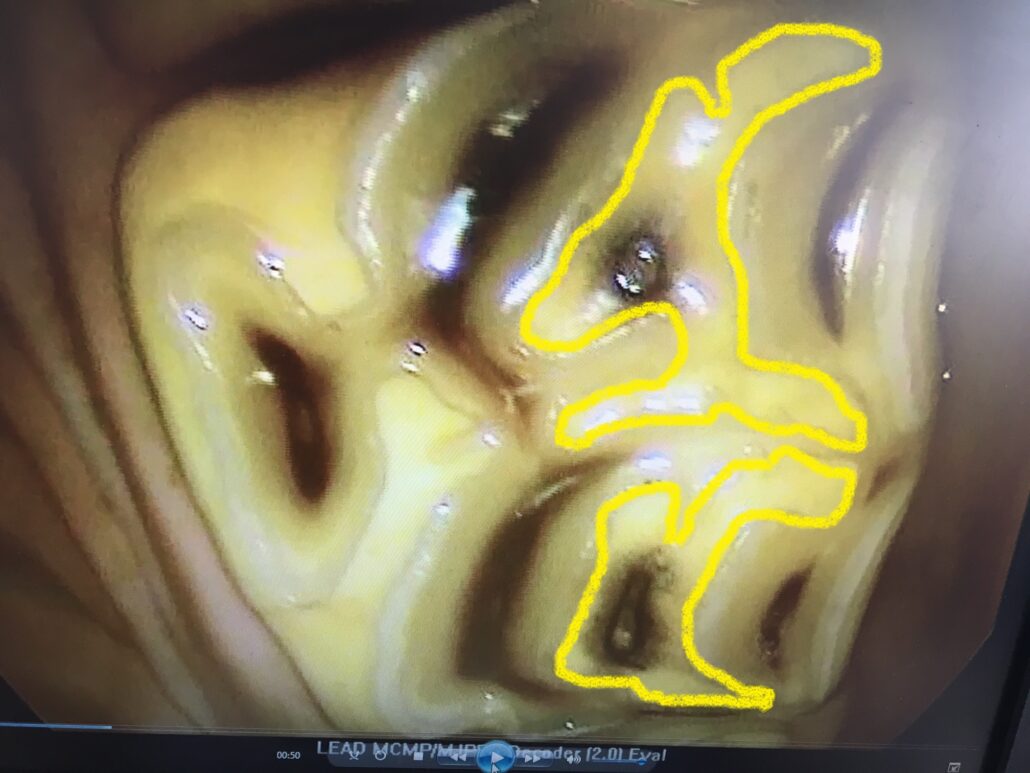
Regular dental examinations using a mirror, or an oral camera, enables us to visualise the surface of the teeth and detect these small but significant defects. Once detected, they can be investigated by probing and/or x-ray to determine the depth of the hole and the requirement for filling.

These holes can easily be filled, much like if you or I went to the dentist! Under standing sedation at our clinic, these holes are thoroughly cleaned out of all the rotten food and filled using a material that binds to the tooth. Once the hole has been filled, food can no longer become trapped and the tooth is no longer at risk of becoming infected or fracturing.
If you have any concerns regarding your horses dental health, please phone our clinic and ask to speak to one of our friendly team who can point you in the right direction!