Pet obesity came to people’s attention about a decade ago, and statistics undeniably show that obesity is on the rise. It has reached epidemic status in the UK!
As veterinarians we are urging pet owners to take excessive weight gain and obesity in pets seriously. We believe obesity is a serious welfare issue in pets because it shortens their life and makes them more likely to develop disease, particularly weight-related disorders. It can cause suffering and can be extremely disabling, affecting your pet’s ability to do their normal activities, like exercise.
Health problems caused by pet obesity
Pet obesity can cause serious health problems, and make existing problems worse, which can reduce the length and quality of your pet’s life. It puts them at greater risk of conditions such as:
- Diabetes
- Heart disease
- Respiratory issues (breathing problems)
- High blood pressure (hypertension)
- Cancers
- Osteoarthritis and a faster degeneration of affected joints
- Urinary bladder stones
On the other hand, obesity may be an indicator of disease, such as hypothyroidism (an underactive thyroid gland) or Cushing’s disease (overactive adrenal glands).
Is your pet at risk of obesity?
Several factors can make obesity more likely in your pet. For example, in dogs:
- Breed – certain breeds have a higher risk.
- Age – the risk increases with age.
- Neuter status – neutered animals are more likely to gain weight if their diet is not managed carefully.
- Sex – apart from older dogs, obesity is reported to be more common in females.
- Obese owner – may lead to having an obese dog as it may be exercised less, or less able to recognise obesity.
Other animals have similar risk factors for obesity.
Does your pet need to lose weight?
Obesity is when your pet has too much body fat and it has a negative impact on their health, welfare and quality of life. Extra body weight and extra body fat tend to go hand in hand, so most overweight dogs will have excess body fat.
Body weight is easy to measure when assessing if your pet is overweight or obese – easier than trying to measure body fat. Using body weight as a guide, pets are considered to be overweight when they weigh 10-20% above their ideal body weight. They are considered obese when they weigh 20% or more above their ideal body weight.
It can be difficult to recognise if your pet is overweight, particularly if it happens slowly or if they have always been overweight. As a pet owner it’s important to understand that weight gained slowly is just as deadly as weight gained rapidly! By recognising weight gain early, your chances of preventing weight-related diseases and severe obesity are greatly improved.
Of course, the best way to check is to take them to the vet and get them properly weighed. However, there are some home methods you can try first, to judge if a trip to the vet is necessary.
Here are some signs to look out for in both cats and dogs:
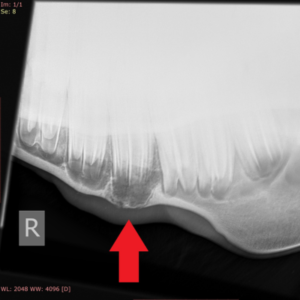
- Ribs – Overweight pets have a layer of fat covering their ribs, which makes them difficult to see or even feel.
- Spine – A ‘fat pad’ will cover their back.
- Tummy – Your pet’s tummy will bulge out and sag downwards, which may wobble or sway when they move
- Face, legs and neck – Obese cats and dogs can get fat pads in these areas.
If your pet doesn’t pass these checks, or if you’re in any doubt, consult your vet. They’ll be able to give your dog a health check and will recommend a weight reduction programme if they think it’s necessary.
In contrast, underweight cats and dogs will have highly visible ribs, hipbones, and backbone. There will be a complete absence of fat around these areas, with an exaggerated waistline and non-existent tummy.
Tips for weight loss and preventing pet obesity
Once you have identified that your dog is overweight or obese, it is important to act to help them to lose weight.
The best approach to weight loss is one that promotes fat loss while preserving lean muscle mass. When pets properly lose fat and gain muscle, pet owners often report an increase in activity levels, enthusiasm and playfulness.
Here are our tips on how you can help your pet in the quest to attain a healthy weight in five easy steps:
1. Food and portion control
Use a specific nutritional product designed for healthy and safe weight loss i.e. one that has lower overall calorie density yet maintains an appropriate nutrient balance. And make sure that you are feeding them the right amount…
Every complete pet food in the UK must have feeding guidelines, but these are based on an assumed activity level, typically above the level of exercise the average cat or dog gets. Plus pets need different amounts of food during their life stage and different breed sizes have different needs, so you need to adjust the recommended feeding amount for your specific pet. When changing their food, portion or feeding pattern, closely monitoring any weight changes over the first few weeks and adjust feeding accordingly.
2.Exercise
There are so many benefits of regular exercise for your pets. Not only will exercise help your pet shed extra pounds, but it will also strengthen respiratory and circulation systems, and aid digestion. The key is to get your pet moving each day, ideally for a minimum of 30 mins (if your pet is able). For some pets e.g. brachycephalic (short nosed) breeds or older pets you will need to tailored exercise to what they are capable of and build up to longer walks slowly. Using an activity tracker can help you to know exactly how much you are both doing!
Cats don’t tend to go on long walks the same way dogs will, making increasing exercise a bit trickier. Try playing interactive games with your cat, with a feather or toy mouse for instance, and feed them on elevated surfaces and in different locations around your home. Keeping these play sessions regular can help to bond with your kitty, whilst keeping them entertained and trim. You could also consider remote-controlled toys and self-directed interactive toys that use technology to engage your pet’s play drive.
3.Treats
Snacks and treats should make up no more than 10% of your dog’s daily calorie intake. Many pet owners feed the proper amount of food but sabotage their efforts by adding one or two snacks throughout the day. As few as 30 extra calories per day means your pet could gain over three pounds in a year. Fresh or frozen green beans, broccoli, and cauliflower all make excellent snacks if approved by your vet. Whatever treats you give, be sure to count those additional calories.
When it comes down to it, most dogs would prefer extra attention to more treats. Spending more time with your pooch will give you both more satisfaction than a treat which is inhaled in an instant and quickly forgotten. But if you do want to reward good behaviour with a treat then break it into smaller pieces and offer them whenever your pet earns it. After all dogs don’t do division!
4. Regular weigh-ins
Monthly weigh-ins are an important component of successful weight loss, and it keeps everyone accountable. It is important to verify weight loss, to ensure that weight loss is neither too rapid nor excessive, and to determine when enough weight has been lost.
5. Look for diseases and get them treated
Although most of the weight gain in cats and dogs is caused by over-feeding and not enough exercise, there are some medical conditions that can contribute to obesity in pets. Fortunately, most of these diseases and illnesses can be treated by a vet, so it’s important to keep an eye on your pet for any changes.
An unexplained increase or decrease in appetite or weight could be a sign of something more sinister. So, be sure to get them checked out by your vet to be on the safe side.
Whatever your weight loss approach, keep in mind the goal is to improve health and prolong life, not just skinny pets. Weight loss done correctly can improve quality of life and extend longevity in pets.
What happens when you reach your weight loss goal?
Weight loss isn’t a single battle; it’s a lifelong war. Once an ideal body weight and condition has been achieved, it is important to maintain that weight. Yo-yo weight loss and gain is no healthier for pets than for humans. The goal is to change your lifestyle so that an active, healthy lifestyle becomes normal.
Follow-up care with your vet is essential for sustained success. Your vet team can help you find an appropriate food and portion for weight maintenance. We recommend tracking your pet’s weight every one to three months to make sure they stay inside the healthy range.