CASE STUDY: TILLY’S ELECTRICAL CARDIOVERSION (TVEC)
Tilly was seen by our vet Kai during a routine yard visit for her annual vaccination. During this visit it was noted that Tilly had a very irregular heart rhythm. Tilly was consequently bought to our clinic for further investigations including blood tests and an ECG to measure the electrical activity of the heart.
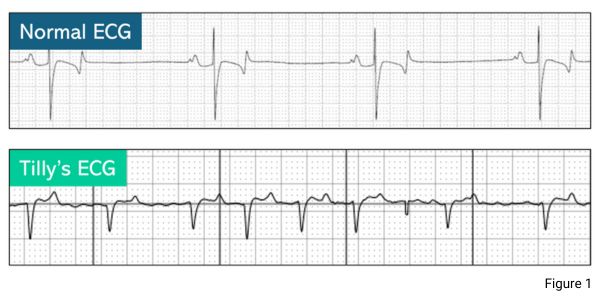
The ECG showed Tilly had a condition called atrial fibrillation. This is where the upper chambers of the heart (the atrium) beat abnormally fast and erratically. You can observe from the ECG traces how Tilly’s heart compares to that of a normal horse (Figure 1).
Atrial fibrillation can cause symptoms including poor performance, exercise intolerance, weakness and collapse. Amazingly, in Tilly’s case she had none of these symptoms at the time, so it was very fortunate we picked up the abnormality early!
ELECTRICAL CARDIOVERSION (TVEC)
Treatment for this condition can include medical therapy or the more preferred treatment choice of electrical cardioversion (TVEC), a procedure performed under a short general anaesthetic that converts the atrial fibrillation to a normal heart rhythm.
We worked alongside medicine specialists Mark Bowen and Gayle Hallowell to perform the procedure at our clinic. Tilly’s arrhythmia was treated the using the TVEC procedure, and we were all delighted when her heart converted to a normal rhythm on the first attempt.

TILLY
Tilly recovered wonderfully from the procedure and was able to return home the next day. During a recent visit, Kai performed a follow-up auscultation and confirmed that Tilly’s heart rhythm remains perfectly normal after treatment! She is now back out and about enjoying her hacking, fun rides and even the odd trip to the gallops!
Thank you to Tilly’s owner who has been wonderful throughout and for her generosity in allowing us to share her story.